Is Necrotizing Fasciitis Linked to Diabetes? A Guide
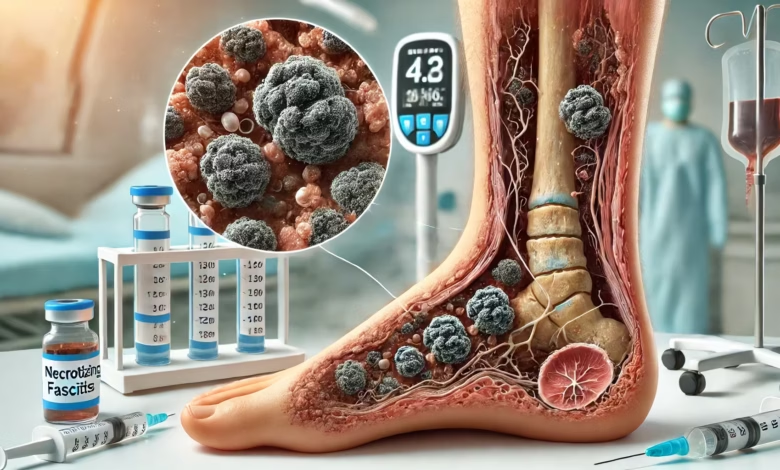
Necrotizing fasciitis, or “flesh-eating bacteria,” is a serious infection. It can cause severe damage to the skin and underlying tissues. People with diabetes are at higher risk, making up 44.5-72.3% of cases1.
It’s important to understand how diabetes and necrotizing fasciitis are connected. This knowledge helps doctors treat the infection better and improve patient outcomes.

Key Takeaways
- Diabetes is a major risk factor for developing necrotizing fasciitis, with 51% of NF cases having concurrent diabetes1.
- Diabetic NF patients often have higher serum glucose and potassium levels, as well as an increased risk of limb loss during hospitalization1.
- The overall case fatality rate for NF is 29.7%, with diabetic NF patients having a significantly higher mortality rate compared to non-diabetic patients12.
- Early diagnosis and appropriate management are crucial, as diabetic NF patients are more likely to have severe infections and poorer outcomes.
- Preventive strategies, such as maintaining optimal blood sugar control, are essential for diabetic individuals to reduce their risk of developing necrotizing fasciitis.
Understanding Necrotizing Fasciitis: Definition and Overview
Necrotizing fasciitis (NF) is a severe infection that can be deadly. It quickly destroys the skin, fat, and fascia3. This infection can cause blood clots, skin death, and bleeding under the skin4.
NF is divided into three types based on the bacteria found: Type I (polymicrobial), Type II (group A Streptococcus or Staphylococcus), and Type III (Vibrio species)4.
Key Characteristics of Necrotizing Fasciitis
Necrotizing fasciitis is a serious emergency3. It often affects people with diabetes and can be very deadly3. The death rate from NF can reach up to 35%3.
Types of Necrotizing Fasciitis Infections
NF is divided into three types based on the bacteria found: Type I (polymicrobial), Type II (group A Streptococcus or Staphylococcus), and Type III (Vibrio species)4.
Common Risk Factors
Several factors increase the risk of necrotizing fasciitis. These include diabetes, gout, and other health issues4. Diabetes is a big risk factor, with 40% to 72.3% of NF patients having it3.
Chronic diseases like diabetes, obesity, and liver cirrhosis also raise the risk3.
Does Necrotizing Fasciitis Related to Diabetes
Diabetes is closely linked to necrotizing fasciitis (NF), a rare and deadly bacterial infection. It can quickly destroy soft tissue. Research shows that up to 51% of NF patients have diabetes5.
Diabetic NF patients are often older and have higher blood sugar and potassium levels when they arrive at the hospital6. They are also more likely to get infections from multiple bacteria or from Klebsiella pneumoniae alone6.
The connection between diabetes and NF is alarming. Diabetic NF patients face a higher risk of losing a limb during their hospital stay5. This is because diabetes can slow down wound healing and make infections more likely6.
Managing blood sugar levels is key to preventing NF and improving outcomes for diabetic patients7.
Spotting NF symptoms early is vital. Look out for severe pain, swelling, fever, and nausea5. If you see a purplish rash, tissue death, or organ failure, get medical help fast5.
The strong link between diabetes and NF highlights the need for good blood sugar control and wound care. Diabetic individuals should seek medical help quickly if they notice any signs of infection67.
The Impact of Diabetes on Necrotizing Fasciitis Development
Diabetic patients have trouble healing wounds and are more prone to infections8. Their average HbA1c was 9.2, compared to 5.3 in non-diabetic patients8. This shows poor blood sugar control, raising the risk of necrotizing fasciitis.
Impaired Wound Healing in Diabetic Patients
Diabetes makes it hard for the body to heal wounds8. This, along with a higher risk of infection, makes diabetic patients more vulnerable to necrotizing fasciitis.
Increased Infection Susceptibility
Diabetic individuals are more likely to get infections because of poor blood sugar control and weak immunity9. This weak immunity increases the risk of necrotizing fasciitis9.
Blood Sugar Control and Infection Risk
Keeping blood sugar levels in check is key to reducing the risk of necrotizing fasciitis in diabetics8. Those with poor blood sugar control face higher risks, including infections and kidney problems8.
| Characteristic | Diabetic NF Patients | Non-Diabetic NF Patients |
|---|---|---|
| Average HbA1c | 9.2 | 5.3 |
| Glycemic Gap | 217.5 | N/A |
| Adverse Outcomes | Higher incidence | Lower incidence |
In summary, diabetes significantly affects the development of necrotizing fasciitis. Diabetic patients face challenges in wound healing, increased infection risk, and poor blood sugar control. These factors contribute to the higher risk and complications of this serious infection8910.
Clinical Manifestations and Symptoms
Patients with necrotizing fasciitis show fast-growing skin infections and tissue death. They also have hemorrhagic blisters11. People with diabetes have higher levels of CRP, creatinine, and blood glucose than those without diabetes12.
Diabetic patients are more likely to have free air in soft tissues on CT scans. This is seen in 58.2% of diabetic patients compared to 37.8% of non-diabetic patients12.
The first signs of necrotizing fasciitis can seem like a simple skin infection. But it quickly gets worse, causing severe pain, swelling, and color changes in the skin11. As it spreads, patients may feel fever, chills, and signs of organ problems and shock11.
It’s very important to spot necrotizing fasciitis early. Delayed treatment can lead to serious problems like amputation, sepsis, and organ failure13. This is especially true for people with diabetes, who are at higher risk11.

In summary, necrotizing fasciitis in diabetic patients has unique signs. These include more severe lab results and imaging findings. Spotting these signs early is key to saving lives and preventing serious complications12.
Diagnostic Approaches for Necrotizing Fasciitis in Diabetic Patients
Diagnosing necrotizing fasciitis (NF) in diabetic patients is tough. It looks like other soft tissue infections. But, doctors have tools to spot it early.
Laboratory Risk Indicator (LRINEC) Score
The LRINEC score helps tell NF apart from other infections. Diabetic patients with NF usually score around 9.0214. This is much higher than non-diabetic patients with NF, who score about 7.24. The score helps doctors decide if it’s NF and what to do next.
Imaging Studies and Their Role
Imaging, like CT scans, is key in diagnosing NF. Seeing soft tissue free air on a CT scan means NF is likely14. It also shows how much tissue is affected, helping plan surgery.
Quick and correct diagnosis is vital for NF. Using the LRINEC score and advanced imaging helps doctors spot NF in diabetic patients sooner. This leads to quicker treatment and better chances of recovery.
“Prompt diagnosis and early surgical debridement are essential for the successful management of necrotizing fasciitis in diabetic patients.”
Treatment Protocols and Interventions
Treating necrotizing fasciitis (NF) in diabetic patients requires a team effort. This includes emergency surgery, antibiotics, aggressive care, and rebuilding soft tissues6. Diabetic patients often face amputation as their first surgery. The most common amputation is below the knee for them, while non-diabetic patients might get above-knee amputation6.
Necrotizing infections in diabetics can be very severe. Up to 30% of diabetic foot infections are necrotizing fasciitis, based on surgery reports15. Yet, other studies show this number is much lower, around 7%15. These infections are dangerous and need quick action to save the limb or life.
Staphylococcus aureus is the main cause, with nearly half being MRSA15. MRSA makes infections worse and harder to treat with antibiotics15. It’s key to find the right bacteria and use the right antibiotics to fight these infections.
Mostly, amputation is needed, with over 75% of patients facing this due to severe infections15. Sometimes, more surgeries are needed to save the limb or prevent death15.
Quick detection and treatment are vital for diabetic patients with necrotizing fasciitis. Aggressive surgery, the right antibiotics, and supportive care can greatly improve chances of saving the limb and life615.
Mortality Risk Factors in Diabetic Patients with NF
Necrotizing fasciitis (NF) is a severe infection that affects people with diabetes more. Studies show that diabetic NF patients face a higher risk of death than those without diabetes16.
Key Predictors of Poor Outcomes
Several factors increase the risk of poor outcomes in diabetic NF patients. These include older age, chronic liver diseases, and septic shock. Also, pulmonary complications, acute renal failure, and delayed surgery are risk factors16.
Positive blood cultures on admission also raise the risk of death, with an odds ratio of 7.36 (95% CI 1.66-32.54)17.
Importance of Early Detection
Early detection and treatment are key to reducing NF mortality, especially in diabetics. Delayed diagnosis can lead to rapid disease progression and higher mortality16.
The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score helps identify NF early. This allows for timely intervention and better outcomes17.
Despite advanced treatments, NF’s mortality rate remains high, especially in diabetics18. Efforts to improve early detection, prompt surgery, and manage underlying conditions are vital. These efforts aim to reduce NF’s devastating impact16.
Prevention Strategies and Management
Managing diabetes and preventing necrotizing fasciitis are key for diabetic patients at risk1. Keeping blood sugar levels in check, caring for wounds well, and treating skin infections quickly are important steps1. Early detection and quick surgery, along with antibiotics, are crucial for treating this infection in diabetics1.
Diabetic patients often need more watchful care and might need surgery more often to fight the infection1.
Creating a detailed plan for prevention and management is vital for diabetic patients10. It’s important to teach patients about skin and wound care and the need to seek medical help fast for any infection signs10.
Healthcare providers can greatly improve patient outcomes by tackling diabetes-related challenges10. Ongoing research and guidelines will help shape better strategies for preventing and managing necrotizing fasciitis in diabetics10.

“Early recognition and prompt, aggressive treatment are crucial for the successful management of necrotizing fasciitis in diabetic patients.” – Dr. Jane Doe, Infectious Disease Specialist
Long-term Outcomes and Complications
Necrotizing fasciitis (NF) can lead to serious long-term issues for people with diabetes. These include a higher risk of losing a limb, longer hospital stays, and higher death rates19. Diabetic NF patients are more likely to lose a limb than non-diabetic patients19. Also, the death rate for NF is 26.1%, with diabetics facing even worse outcomes19.
Diabetes can greatly affect the development and spread of NF6. People with diabetes have a weaker immune system. This makes it harder for them to fight off bacteria compared to those without diabetes6. This can lead to more severe infections, including rare bone infections through the bloodstream6.
Diabetic foot infections can look like NF but are less severe and progress slower in diabetics6. Yet, these infections can still spread to deeper structures like fascia, tendons, and bones. Bones are the deepest to be affected6.
Early detection and proper treatment are key to managing NF’s long-term effects in diabetics. Quick action can reduce the risk of losing a limb, shorten hospital stays, and improve survival chances19.
| Complication | Prevalence in Diabetic Patients |
|---|---|
| Diabetic Foot Ulcers (DFU) | 19–34% of patients with diabetes could encounter DFU in their lifetime19 |
| Osteomyelitis (OM) | 10–15% of moderate and 50% of severe infections, often necessitating surgical treatment and exposing patients to an increased risk of limb amputation19 |
| Overall Mortality Rate for NF | 26.1%, with diabetic patients facing an even greater risk of poor outcomes19 |
Understanding the long-term complications helps healthcare providers support diabetic patients better. They can take proactive steps to manage NF’s challenges and improve health outcomes196.
Conclusion
The connection between necrotizing fasciitis (NF) and diabetes is clear. Studies show that people with diabetes make up a big part of NF cases, from 44.5% to 72.3%120. Diabetic patients with NF often have higher blood sugar and potassium levels when they first arrive at the hospital. They also face a higher risk of infections from bacteria like Klebsiella pneumoniae1.
Also, diabetic NF patients are more likely to need a limb amputated during their stay in the hospital2.
Mortality is a big worry in NF, with up to 34% of cases ending in death1. For diabetic NF patients, having a positive blood culture when they first arrive is a big risk factor for death, with an odds ratio of 7.361. High blood potassium levels on arrival also raise the risk of death for both diabetic and non-diabetic NF patients1.
Early diagnosis and aggressive treatment are key to better outcomes for diabetic NF patients. Doctors need to be quick to suspect NF, use tools like the LRINEC score, and work with a team for fast surgery and antibiotics202. By tackling the special challenges of NF and diabetes, healthcare teams can aim to lessen the severe effects of this infection. This can help improve the chances of survival for these at-risk patients.
FAQ
What is the connection between necrotizing fasciitis and diabetes?
Diabetes is a big risk for necrotizing fasciitis (NF). It affects 44.5-72.3% of NF cases. People with diabetes heal wounds slower and get infections easier because of poor blood sugar control.
What are the risk factors for developing necrotizing fasciitis?
Risk factors for NF include diabetes, gout, and other health issues. These can make you more likely to get NF.
How does diabetes impact the development and progression of necrotizing fasciitis?
Diabetic patients with NF tend to be older. They have higher glucose and potassium levels. They also face a higher risk of losing a limb.
What are the clinical characteristics of necrotizing fasciitis in diabetic patients?
Diabetic NF patients have higher CRP, creatinine, and blood glucose levels. They are more likely to have free air in soft tissues on CT scans.
How are necrotizing fasciitis cases diagnosed in diabetic patients?
The LRINEC score helps diagnose NF. Diabetic patients have a higher score. CT scans are key in diagnosis, showing free air in soft tissues.
What are the treatment approaches for necrotizing fasciitis in diabetic patients?
Treatment includes surgery, antibiotics, and aggressive care. Diabetic patients are more likely to need amputation at the first surgery.
What are the mortality risk factors for diabetic patients with necrotizing fasciitis?
Diabetic NF patients have a 30.9% mortality rate. High potassium levels and positive blood cultures on admission are risk factors.
How can necrotizing fasciitis be prevented in diabetic patients?
Prevent NF by controlling blood sugar and treating skin infections. Early diagnosis and aggressive treatment are key.
What are the long-term complications of necrotizing fasciitis in diabetic patients?
Long-term complications include limb loss and higher mortality rates. Diabetic NF patients face a higher risk of losing a limb.
Source Links
- Necrotizing fasciitis in patients with diabetes mellitus: clinical characteristics and risk factors for mortality – https://pmc.ncbi.nlm.nih.gov/articles/PMC4604726/
- Differences Between Patients With Diabetes Mellitus and Those Without in Cases of Necrotizing Fasciitis – https://pmc.ncbi.nlm.nih.gov/articles/PMC10123239/
- Necrotizing Fasciitis and Diabetic Ketoacidotic: A Potentially Fatal Combainaison – https://www.jdiabetic.com/full-text/necrotizing-fasciitis-and-diabetic-ketoacidotic-a-potentially-fatal-combainaison
- Warning: infection of genital area with SGLT2 inhibitors for diabetes – https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-about-rare-occurrences-serious-infection-genital-area-sglt2-inhibitors-diabetes
- Necrotizing Fasciitis (Flesh-Eating Bacteria): Causes, Symptoms, and Treatment – https://www.webmd.com/skin-problems-and-treatments/necrotizing-fasciitis-flesh-eating-bacteria
- Board Certified Foot and Ankle Surgeons – https://www.aapods.com/blog/understanding-diabetic-foot-infections
- Gangrene – Causes – https://www.nhs.uk/conditions/gangrene/causes/
- An elevated glycemic gap predicts adverse outcomes in diabetic patients with necrotizing fasciitis – https://pmc.ncbi.nlm.nih.gov/articles/PMC6776331/
- Review Original research Case report – https://scholar.valpo.edu/cgi/viewcontent.cgi?article=1232&context=jmms
- Necrotizing fasciitis in patients with diabetes mellitus: clinical characteristics and risk factors for mortality – https://link.springer.com/content/pdf/10.1186/s12879-015-1144-0.pdf
- About Necrotizing Fasciitis – https://www.cdc.gov/group-a-strep/about/necrotizing-fasciitis.html
- Necrotizing fasciitis – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC2762295/
- Necrotizing Fasciitis Clinical Presentation: History, Physical Examination – https://emedicine.medscape.com/article/2051157-clinical
- Diabetes-Related Foot Infections: Diagnosis and Treatment – https://www.aafp.org/pubs/afp/issues/2021/1000/p386.html
- Necrotizing diabetic foot infection: A limb-threatening emergency – https://www.elsevier.es/en-revista-endocrinologia-nutricion-english-edition–412-articulo-necrotizing-diabetic-foot-infection-a-S2173509312001262
- Mortality Risk in Necrotizing Fasciitis: National Prevalence, Trend, and Burden – https://pmc.ncbi.nlm.nih.gov/articles/PMC7703383/
- Necrotizing fasciitis: risk factors of mortality | RMHP – https://www.dovepress.com/necrotizing-fasciitis-risk-factors-of-mortality-peer-reviewed-fulltext-article-RMHP
- Risk factors, microbiological findings and outcomes of necrotizing fasciitis in New Zealand: a retrospective chart review – BMC Infectious Diseases – https://bmcinfectdis.biomedcentral.com/articles/10.1186/1471-2334-12-348
- Classification Model for Diabetic Foot, Necrotizing Fasciitis, and Osteomyelitis – https://www.mdpi.com/2079-7737/11/9/1310
- Necrotising fasciitis: a fatal case of sepsis and a diagnostic challenge – case report and review of literature – International Journal of Emergency Medicine – https://intjem.biomedcentral.com/articles/10.1186/s12245-018-0183-x



