How Hyperthyroidism Causes AFib: Understanding the Connection

The thyroid gland has an outsized effect on heart health, especially when it’s overactive. Hyperthyroidism speeds up bodily processes, often causing irregular heart rhythms like atrial fibrillation (AFib). But how exactly does this happen? Higher levels of thyroid hormones increase the heart rate, compromise electrical stability, and elevate the risk of AFib, making it a common complication for those with hyperthyroidism. Understanding this connection is essential to managing both conditions effectively.
Understanding Hyperthyroidism
Hyperthyroidism occurs when your thyroid gland produces excessive levels of thyroid hormones, disrupting normal bodily functions. This condition not only impacts metabolism but can also have far-reaching effects on the heart, making early understanding and management crucial. Let’s break it down further.
Definition and Causes of Hyperthyroidism
Hyperthyroidism, or an overactive thyroid, happens when the thyroid produces more hormones than your body needs. These hormones, primarily T3 (triiodothyronine) and T4 (thyroxine), regulate metabolism, but in high amounts, they speed up many body systems.
Common causes include:
- Autoimmune Conditions: Graves’ disease is the leading cause of hyperthyroidism. It occurs when your immune system mistakenly attacks the thyroid gland, causing it to overproduce hormones. Learn more about Graves’ disease and hyperthyroidism.
- Nodular Thyroid Disease: Toxic nodular goiter or a single overactive thyroid nodule can stimulate excess hormone production.
- Thyroiditis: This inflammation might release an excess of stored hormones into your bloodstream. Thyroiditis can be triggered by infections, postpartum changes, or certain medications. Get deeper insights into overactive thyroid causes here.
Symptoms of Hyperthyroidism
Recognizing hyperthyroidism starts with being aware of its symptoms, which may vary between individuals. These symptoms often appear gradually but can significantly disrupt day-to-day life.
Key signs to watch for include:
- Unintentional Weight Loss – Even if your appetite increases, the accelerated metabolism burns calories rapidly.
- Rapid or Irregular Heartbeat – Known as tachycardia, this symptom may feel like your heart is racing, even during rest. This is a critical concern since unchecked hyperthyroidism can lead to conditions like atrial fibrillation (AFib). Understand hyperthyroidism symptoms here.
- Increased Appetite – It might feel like you’re eating constantly without any weight gain.
- Nervousness or Anxiety – The heightened hormone levels can mimic chronic stress or anxiety.
- Excessive Sweating and Heat Sensitivity – You may feel warmer than usual due to an overactive metabolism.
Other possible symptoms include shaky hands, sleep problems, and muscle weakness. Pay close attention if multiple symptoms appear together.
Diagnosis of Hyperthyroidism
Diagnosing hyperthyroidism involves several steps to ensure accuracy. Physicians rely on a combination of medical history, physical exams, and lab tests.
Here’s how it’s typically done:
- Blood Tests: These tests measure levels of thyroid-stimulating hormone (TSH) and thyroid hormones (T3 and T4). Low TSH with elevated T3 or T4 often confirms the diagnosis. Explore diagnostic measures for hyperthyroidism.
- Radioactive Iodine Uptake (RAIU): This test evaluates how much iodine your thyroid absorbs, helping differentiate between causes like Graves’ disease or nodular thyroid disease.
- Thyroid Scans: Imaging techniques provide a visual of the thyroid gland, identifying nodules or structural abnormalities. Details on diagnostic imaging available here.
Accurate diagnosis is critical for effective treatment. Once identified, personalized therapy can mitigate risks such as AFib and other complications.
What is Atrial Fibrillation (AFib)?
Atrial Fibrillation, often referred to as AFib, is one of the most common heart rhythm disorders. At its core, AFib interferes with the heart’s ability to beat in a regular, coordinated manner, leading to several health risks. To understand its effects and implications, let’s explore its definition, mechanism, symptoms, and potential long-term dangers.
Definition and Mechanism of AFib
Atrial Fibrillation is a type of arrhythmia, or irregular heartbeat. It occurs when the heart’s upper chambers (atria) beat chaotically and out of sync with the lower chambers (ventricles). This irregular rhythm can range from occasional episodes to chronic, continuous irregularity.
Why does this happen? Normally, the heart’s rhythm is governed by electrical signals that move in an orderly fashion. In AFib, these signals become erratic, disrupting the regular heartbeat. Think of it like faulty wiring causing inconsistent flickers in a light bulb—a lack of coordination leads to inefficiency. This irregular signaling can reduce the heart’s ability to pump blood effectively, which may result in poor circulation.
AFib isn’t just a benign irregularity. It can cause the heart to beat too quickly, too slowly, or unpredictably, putting undue stress on the heart over time. According to the American Heart Association, this condition can lead to blood clots, strokes, and other cardiovascular issues if left untreated.
Symptoms and Risks of AFib
AFib symptoms can range from mild to severe, depending on the individual. For some, it may feel like a slight flutter in the chest, while others could experience overwhelming fatigue or chest pain. Here are some common signs to watch for:
- Heart Palpitations: A racing, fluttering, or irregular heartbeat is often one of the first signs of AFib.
- Shortness of Breath: Especially during physical activity or even at rest, this symptom signals reduced blood flow.
- Fatigue: Persistent tiredness can result from an inefficient heart struggling to pump blood.
- Lightheadedness or Dizziness: A lack of proper circulation may lead to feeling faint.
- Chest Discomfort: This may range from mild pressure to sharp pain, especially during AFib episodes.
The risks of AFib go beyond uncomfortable symptoms. The condition significantly increases the likelihood of serious complications:
- Stroke: Blood clots can form in the poorly contracting atria, which can travel to the brain and block blood flow. AFib patients are five times more likely to suffer a stroke, notes the Cleveland Clinic.
- Heart Failure: Over time, the heart may struggle to meet the body’s demands, leading to fluid buildup and reduced cardiac function.
- Chronic Fatigue: Constant inefficiency in pumping blood can leave you feeling perpetually drained.
AFib isn’t always easy to recognize as symptoms may overlap with other conditions, or episodes can occur without obvious signs. This makes regular medical evaluations essential, especially for those at higher risk due to factors like age, underlying heart disease, or thyroid disorders. Learn more about AFib symptoms and risks from Mayo Clinic.
Recognizing these symptoms early and understanding the associated risks can lead to timely intervention, which may prevent severe complications down the line. Following appropriate medical guidance is crucial for effective management.
The Connection Between Hyperthyroidism and AFib
Hyperthyroidism and atrial fibrillation (AFib) often occur together. Studies repeatedly show a significant overlap, underlining the need to understand their connection. Hyperthyroidism ramps up metabolic processes and can overstimulate the heart, often leading to irregular heartbeats and AFib. Let’s explore the prevalence of this relationship and the mechanisms behind it.
Prevalence of AFib in Hyperthyroidism
How common is AFib in individuals with hyperthyroidism? Various studies highlight a striking connection. Atrial fibrillation occurs in 5% to 15% of hyperthyroid patients, far above its incidence in the general population, which is approximately 1% to 3% according to research (Kostopoulos, 2024). Some studies, like a review published in ScienceDirect, report even higher variability, with estimates ranging from 16% to 60% in hyperthyroid cases (Reddy, 2017).
Even more focused research reveals intriguing patterns:
- AFib is often more prevalent in older hyperthyroid patients due to cumulative cardiac strain over time.
- Men with hyperthyroidism show slightly higher AFib risk compared to women.
A detailed analysis published in the JAMA Internal Medicine journal found that 8.3% of patients with diagnosed hyperthyroidism developed AFib within 30 days (Frost, 2004). This data underlines the importance of early intervention when thyroid imbalances are identified.
Mechanisms Linking Hyperthyroidism to AFib
What physically ties an overactive thyroid gland to chaotic heart rhythms? The answer lies in how thyroid hormones influence cardiac systems. Here’s what happens:
- Increased Heart Rate: Elevated thyroid hormones (T3 and T4) stimulate the heart to beat faster, mimicking the effects of adrenaline. Hyperthyroidism reduces cardiac electrical stability, setting the stage for AFib.
- Enhanced Atrial Electrical Excitability: Studies suggest that excess thyroid hormones activate arrhythmogenic foci, small clusters of cells in the heart that disrupt the normal rhythm (Bielecka-Dabrowa, 2009).
- Elevated Cardiac Output: With hyperthyroidism, the heart pumps blood faster and harder. This sustained effort increases atrial pressure and size over time, promoting structural remodeling—a key precursor to AFib.
- Altered Cellular Signaling: Hyperthyroidism may enhance autoantibodies targeting β1-adrenergic and M2-muscarinic receptors, both crucial for regulating heart rate (Reddy, 2017).
The clinical picture becomes more complex when these factors combine. Elevated thyroid hormones can cause both abnormal electrical activity and physical enlargement of the atria, making the heart susceptible to rhythm disturbances. Evidence from the American Heart Association also suggests that thyroid-related AFib is often reversible once thyroid function normalizes, but the process may take months (Kostopoulos, 2024).
Understanding these mechanisms not only clarifies how hyperthyroidism causes AFib but also highlights the importance of treating thyroid imbalances as part of cardiac care.
Physiological Mechanisms
Hyperthyroidism significantly impacts the heart through various physiological mechanisms. The overproduction of thyroid hormones disrupts normal cardiac function, contributing to irregular heart rhythms like atrial fibrillation (AFib). Understanding these changes requires examining how thyroid hormones influence the heart’s electrical and structural systems.
Effects of Thyroid Hormones on the Heart
Thyroid hormones, specifically T3 and T4, drastically alter heart function. These hormones regulate energy metabolism, and their excessive levels in hyperthyroidism overstimulate the heart.
Key effects on the heart include:
- Increased Resting Heart Rate: Elevated thyroid hormone levels raise the heart rate, often causing tachycardia. This consistent pacing strain can destabilize the heart’s rhythm.
- Enhanced Electrical Activity: Overactive thyroid hormones boost electrical excitability in the heart’s atria (upper chambers). This increase can create irregular rhythms, setting the conditions for AFib.
- More Cardiac Output: Hyperthyroidism causes the heart to work harder, pumping more blood per beat due to increased contractility—how strong each heartbeat is.
Imagine your heart as an engine running at full throttle without rest. This relentless activity overstretches the system, leading to complications like AFib. According to Harvard Health, thyroid hormones directly influence the heart’s pace and force, creating long-term excess strain.
Further research supports this link. A study in the National Library of Medicine highlights how hyperthyroidism affects heart rate and myocardial (heart muscle) activity, often leading to arrhythmias (PubMed).

Photo by Tara Winstead
Impact on Cardiac Remodelling
Beyond electrical disturbances, hyperthyroidism can reshape heart structures, a process called cardiac remodeling. This refers to physical and molecular changes in the heart caused by excessive thyroid hormones.
Key remodeling effects include:
- Atrial Enlargement: As the heart works harder to meet increased metabolic demands, atrial chambers stretch and enlarge. Over time, this structural change escalates the risk of developing AFib.
- Hypertrophy (Thickened Heart Walls): Hyperthyroid-induced hypertension (high blood pressure) may thicken heart walls, reducing its capacity to pump efficiently.
- Fibrotic Tissue Development: Excessive thyroid hormones amplify signals like angiotensin II, promoting scar-like tissue in the heart. This stiffens the heart muscle and disrupts rhythm.
Cardiac remodeling in hyperthyroidism isn’t just theoretical—clinical studies back its occurrence. According to Endocrine Society research, the hyperthyroid state fosters structural changes, leading to symptoms like low exercise tolerance and irregular heartbeats. This remodeling creates a fertile ground for arrhythmias like AFib to flourish.
While these effects often diminish as thyroid levels stabilize, the heart may retain some damage, underscoring the need for early intervention.
Diagnosis of AFib in Hyperthyroid Patients
Atrial fibrillation (AFib) is commonly diagnosed through a combination of clinical evaluation, symptoms, and targeted testing. In hyperthyroid patients, identifying AFib is particularly significant due to the hormonal effects on the heart. Proper diagnostic tools help differentiate AFib from other possible arrhythmias and lead to effective treatment strategies. Understanding the most reliable techniques for AFib diagnosis is key.
Diagnostic Tests for AFib
When physicians suspect AFib, they rely on both clinical tools and long-term heart monitoring. Modern technology ensures greater accuracy in detecting irregular heartbeat episodes, even those that occur sporadically. Below are the standard tests often conducted:
1. Electrocardiogram (EKG/ECG)
An ECG is the go-to test for diagnosing AFib. By evaluating the electrical activity of the heart, it identifies irregularities in rhythm and rate. Thin wires with tiny electrodes are placed on the chest to record electrical signals for just a few minutes. AFib is evident if there’s a chaotic and rapid rhythm in the atria.
- Why is it crucial? This test gives immediate, clear data on heart function, making it an essential starting point. Learn more from Mayo Clinic.
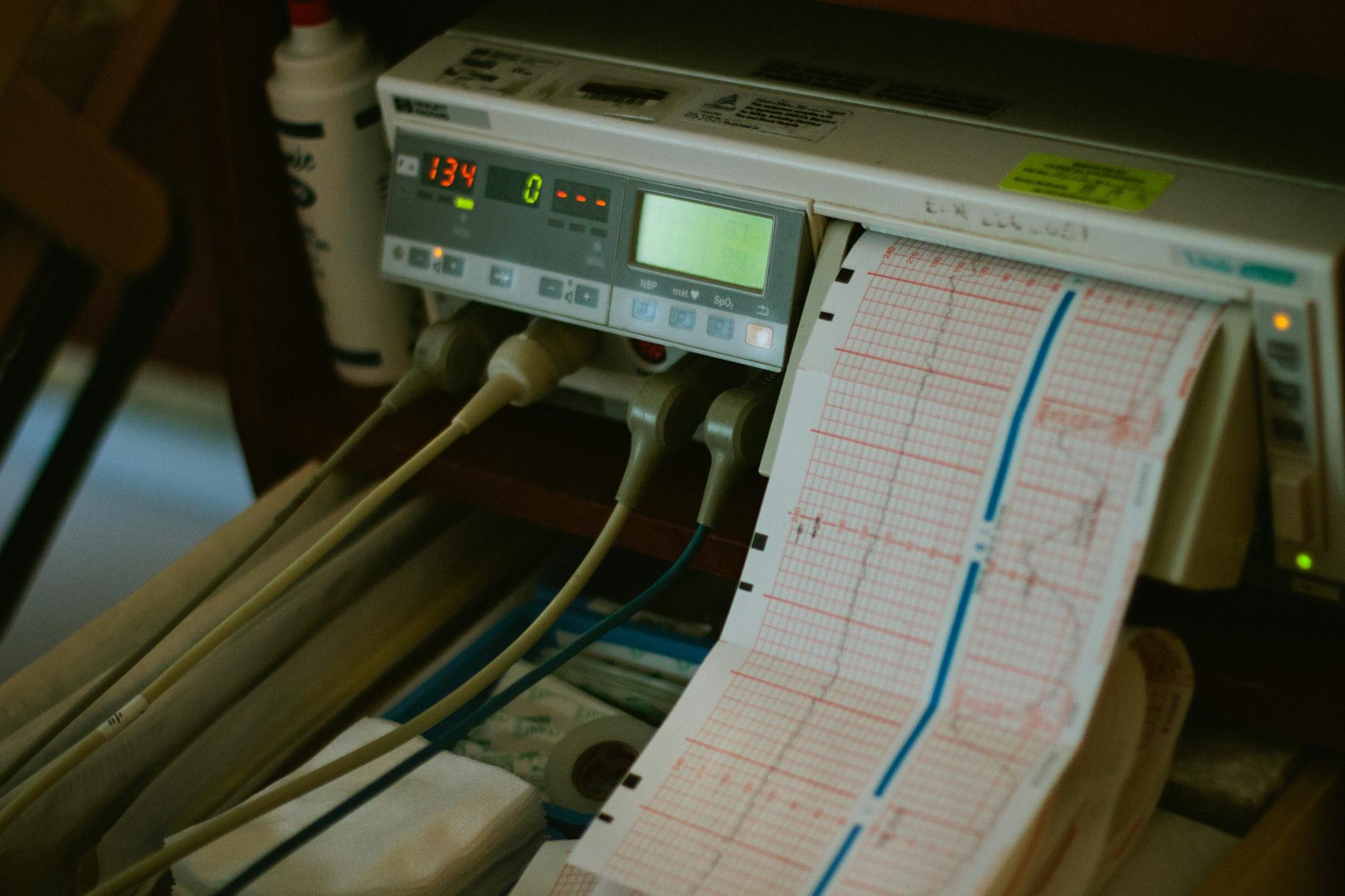
Photo by Pixabay
2. Echocardiogram
Ultrasound imaging of the heart, known as an echocardiogram, produces detailed visuals of its structures and performance. Two variations include:
- Transthoracic echocardiogram: A non-invasive device captures pictures through the chest wall.
- Transesophageal echocardiogram (TEE): Provides clearer images by guiding a small probe down the esophagus, especially useful for spotting blood clots in the atria.
- Benefits in hyperthyroid patients: This test uncovers any structural damage caused by hyperthyroidism, such as atrial enlargement, a common risk factor for AFib. Additional details on echocardiograms here.
3. Long-Term Monitoring (e.g., Holter Monitors)
For cases where AFib episodes are intermittent, continuous monitoring with wearable devices like Holter monitors or event recorders is necessary. These tools track heart activity over 24 to 48 hours—or even weeks—detecting irregular rhythms that might not appear during a short ECG.
- Advanced options: Some patients may require implantable loop recorders for extended monitoring of up to several months. Technologies such as two-lead Holters have proven their utility in identifying paroxysmal (short, sporadic) AFib. Explore long-term monitoring techniques.
4. Blood Tests
A thorough diagnosis often involves thyroid function tests, especially for hyperthyroid patients. Blood tests can confirm abnormal thyroid hormone levels (T3, T4, and TSH), playing a critical role in connecting hyperthyroidism to AFib.
By combining these reliable diagnostic methods, healthcare providers can zero in on AFib while addressing the root causes linked to hyperthyroidism.
Management Strategies
Effective management of hyperthyroidism and AFib involves tailored approaches to address both the underlying thyroid condition and the heart rhythm irregularities. Let’s explore the optimal treatment pathways.
Treating Hyperthyroidism
Managing hyperthyroidism is essential for reducing its cardiac complications, including AFib. Treatment aims to restore normal thyroid hormone levels and may include the following options:
- Medications: Anti-thyroid medications like methimazole and propylthiouracil (PTU) help reduce thyroid hormone production. These drugs are often a first-line treatment, especially for those with less severe symptoms. Patients may need periodic blood tests to monitor thyroid levels and adjust doses accordingly. Learn more about anti-thyroid medications.
- Radioactive Iodine Therapy (RAI): This method uses low-dose radioactive iodine (I-131) to shrink and eventually destroy overactive thyroid tissue. It’s highly effective and minimally invasive, making it a popular choice. While the thyroid gland’s function can permanently decrease after RAI, patients may require lifelong thyroid hormone replacement. Read more on radioactive iodine therapy.
- Thyroid Surgery (Thyroidectomy): Surgery may be necessary for individuals with severe hyperthyroidism, large goiters, or thyroid cancer. While highly effective, it comes with potential risks like damage to adjacent glands. Those undergoing thyroidectomy will also need long-term hormone replacement therapy. Explore thyroid surgical options.
Each treatment option has its considerations, and the choice often depends on the patient’s age, severity of hyperthyroidism, and overall health.
Managing AFib in Hyperthyroid Patients
AFib linked to hyperthyroidism often improves with successful thyroid treatment, but managing the arrhythmia itself is equally important. Common strategies include controlling the heart’s rate and rhythm and reducing the risk of complications like stroke.
- Rate Control Medications: Drugs like beta-blockers (e.g., propranolol) or calcium channel blockers (e.g., diltiazem) slow the heart rate and improve symptoms. Beta-blockers are particularly beneficial in hyperthyroid patients since they also counteract the excessive stimulation of the thyroid hormones. For more on the role of rate control, see this article.
- Anticoagulants: AFib increases clot formation risk, which can lead to a stroke. Anticoagulants like warfarin or newer direct oral anticoagulants (DOACs) are prescribed to prevent clot-related complications. The choice depends on individual stroke risk, often assessed using scoring systems like CHA2DS2-VASC. Explore anticoagulant therapy options.
- Rhythm Control Strategies: In some cases, reverting the heart to a normal rhythm is pursued. Electrical cardioversion (shock therapy) or medications such as amiodarone can help achieve rhythm regularity. However, hyperthyroid-related AFib may spontaneously resolve once thyroid hormones normalize, so rhythm correction is usually delayed until thyroid function is stable. Read a detailed guideline on AFib and rhythm management.
These strategies are often used in combination to achieve the best patient outcomes. A comprehensive plan addressing both thyroid function and AFib is crucial to lower long-term risks.
Key Takeaways
Hyperthyroidism is a condition with far-reaching consequences on heart health, particularly its link to atrial fibrillation (AFib). These are the essential points to understand when exploring how hyperthyroidism causes AFib. These insights summarize the connection and impact of these conditions:
The Role of Thyroid Hormones in AFib
- Excess Hormones Overstimulate the Heart: Hyperthyroidism releases excessive thyroid hormones (T3 and T4). This hormonal surge accelerates the heart rate and disrupts its regular electrical signaling, leading to arrhythmias like AFib.
- Increased Electrical Excitability: High thyroid hormone levels enhance the heart’s electrical activity. This overstimulation often creates the erratic rhythms that typify AFib.
- Physical Changes in the Heart: Persistent overstimulation can enlarge the atria or remodel heart structures, exacerbating the risk of AFib. Learn more about hyperthyroidism impacts on the heart.
Prevalence and Impact of AFib in Hyperthyroid Patients
- Higher Risk in Hyperthyroidism: AFib is present in 5%-15% of hyperthyroid individuals, compared to 1%-3% in the general population (Bielecka-Dabrowa, 2009).
- Reversibility with Treatment: In many cases, AFib associated with hyperthyroidism resolves once thyroid hormone levels stabilize within 4-6 months. However, some heart damage may persist (Kostopoulos, 2024).
Symptoms and Diagnosis
- Common Warning Signs: Symptoms of AFib, including heart palpitations, fatigue, and shortness of breath, often accompany hyperthyroidism. Addressing these early improves outcomes. More on hyperthyroid-linked AFib symptoms here.
- Diagnostic Importance: Tests like ECG, echocardiograms, and thyroid function panels help confirm AFib as a complication of hyperthyroidism. Detailed monitoring further aids in pinpointing irregular episodes.
Management and Outlook
- Dual Treatment Focus: Both the thyroid imbalance and AFib must be managed together. Treatment options, like anti-thyroid medication or rate-control therapies such as beta-blockers, can address symptoms effectively.
- Preventive Care: Timely interventions minimize long-term heart damage, stroke risks, and other complications common in AFib patients.
Understanding this intricate tie between thyroid hormone levels and heart rhythm disruptions can guide effective treatments and potentially reversible outcomes. This knowledge empowers patients and healthcare providers to take early action, reducing risks associated with hyperthyroidism and AFib through comprehensive care.
Conclusion
Hyperthyroidism directly contributes to the development of atrial fibrillation (AFib) by overstimulating the heart. Excess thyroid hormones increase heart rate, amplify electrical activity in the atria, and cause cardiac remodeling, all of which elevate the risk of an irregular heartbeat. This connection underscores the importance of addressing thyroid imbalances promptly.
If you suspect symptoms like a racing heart or fatigue linked to hyperthyroidism, consult a healthcare provider. Timely intervention can help restore thyroid function, potentially reversing AFib and protecting your long-term heart health.